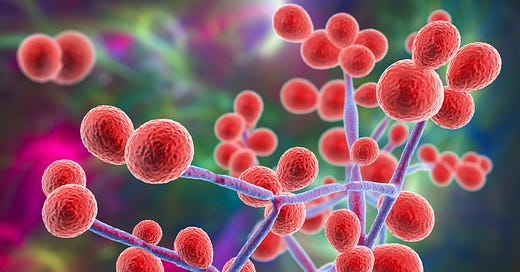
We are hearing more in the news about the concerns of a rapidly spreading fungus, Candida auris. This has been a relatively rare fungal infection, so it is interesting that is now being reported as fast-spreading and something that could become concerning. Let’s look at what we currently know about this strain of fungus and who should be concerned about it.
Candida auris has been typically a hospital acquired infection known to be an issue in U.S. healthcare facilities. A hospital is a place where surfaces and rooms are being constantly treated with antimicrobial substances. This may create a sort of “superbug” environment, which could possibly result in a breeding ground for germs that are difficult to defeat. Candida species have been mentioned as very typical among the known hospital acquired infection. We should also think about the possibility of fungal infections being more likely to occur in people who have a compromised immune system. The concern for those that do get this strain of Candida is that there is no medication at this time that appears effective. This only includes allopathic medications, as no natural remedies were discussed.
According to the Minnesota Department of Health, Candida auris most commonly occurs in those people who have:
Weakened immune systems.
Frequently occurs in health care settings, particularly in long-term acute care hospitals and long-term care facilities that provide ventilator care.
Invasive medical devices such as breathing tubes, feeding tubes, and central venous catheters.
Keep all of this in mind as we look at the recent reporting on Candida auris, published on February 5th in the UK Mirror. This is an article that is sounding the alarm about the spread of Candida Auris in the US. In the article, they discussed the following:
Candida auris is spreading rapidly across the U.S. with Washington state confirming first cases in January 2024. They then contradict this claim by explaining that candida auris first appeared in the U.S. 15 years ago.
They claim that the fungus has a “high fatality rate and spreads easily in medical facilities.” This is not news if they are referring to the high fatality rate in people who may be immune compromised in a medical facility. It does seem to be difficult to treat with anti-fungal medications, but that could also be related to the health status of those who may be in the hospital when they acquired it.
In an article on VeryWellHealth.com, it states the following: “While C. auris infections do not pose a threat to healthy individuals or the general public, it can spread easily in hospitals if standard precautions are not used.”
They go on to say in the article that most serious infections occur in people with serious underlying disease comorbidities. They have other conditions, for example Diabetes Type 2, pneumonia, or other active infections that could compromise their ability to deal with the Candida auris. With this information in mind, should you be concerned about this newly reported spread of this fungus?
For this type of fungus, healthy people with a relatively strong immune system rarely develop serious infections from C. auris. Medical experts familiar with C. auris have stated that it is not a broad threat to the public. That is not the sense that one would get from reading the February 2024 Daily Mirror article. However, the facts are that Candida auris is a known hospital acquired infection and has been around for some time.
Some symptoms include fever, chills, sweating and low blood pressure if the fungus should get into the bloodstream. It is easy to confuse the symptoms of Candida auris with an active bacterial infection. Testing would need to be done to confirm the source of the symptoms.
Keep your immune system strong
What can you do to keep your immune system strong and become more resilient in the face of possible spreading fungal infections?
First, be sure to clean up the gut. Work on healthy and complete digestion. This would mean choosing healthy, unprocessed foods. Remove rich, fatty foods, high protein foods and anything that is highly processed. The foods that are easy to digest and can help the development of a healthy gut microbiome are natural, unprocessed foods that are rich in starches and low in fat. Examples include, potatoes, sweet potatoes, lentils, garbanzo beans, fruits, vegetables and nuts and seeds. All of these natural, unprocessed foods are easy for the body to digest. See more about eating this way in this free download.
Use these 3 key supplements as a way to tune-up your digestive system. The health of your digestive system is connected to the health of your immune system. An important part of our immune defense system, the Peyer’s Patches, are located in the small intestine. Support your digestive wellness and in turn his supports your immune health.
Digestive enzymes with each meal to help the body completely digest and assimilate food. Look for a digestive enzyme that has a variety of enzymes for digesting carbohydrates, fats and proteins.
A good probiotic supplement (one with Lactobacillus acidophilus and Bifidus spp) helps to diminish the chances of candida thriving in the gut. If you ever take any antiobiotic, consider taking a good quality probiotic every day for about 6 months. A healthy gut microbiome is a great protection against candida. A person who has taken rounds of antibiotics (maybe one who is in the hospital…) is much more susceptible to fungal infections.
Gentian or bitters. A small amount of herbal bitters should be taken about 15-30 minutes before a meal to improve stomach acid production and overall digestion.
Natural remedies for fungal infections
In natural medicine, we use these natural remedies to deal with Candida Spp in general (though this is not focused on Candida auris but likely these would be helpful).
Caprylic acid works by interfering with the activity of the cell walls of the fungus. It works to inhibit the growth of all forms of yeast. It effectively thwarts the growth of the infection and helps to release the yeast cells from the intestinal walls.
Oil of Oregano has been found to inhibit the activity of Candida. This could be in part due to the terpenoid phenols in oil of oregano, which include carvacrol, thymol and carvacol. Oil of oregano has found to be effective without creating a resistance in the candida species.
Usnea is a traditional herbal remedy known for its anti-fungal properties. It has a cooling energy and so it is typically used when there are signs of heat, infection and inflammation. These often present as red, itchy and painful symptoms. Interestingly, usnea also has an affinity for the lungs and urinary tract and could be considered for those infections.
Could those that have taken the Covid vaxx be more at risk for Candida auris than others? There has been some discussion that the nature of the vaccine may have a short-circuiting effect on the immune system. Dr. Joseph Mercola wrote and article, published November 24th, 2021 and shared the following:
There was a study that looked at the failure of informed consent in vaccine trial participants. Apparently, volunteers were not told that the vaccine could make them more susceptible to severe disease.
Coronaviruses cause an odd response from the immune system in general. This is concerning because the vaccine also creates this effect because the mRNA instructs your cells to make the SARS-CoV-2 spike protein (S protein). There has been discussion that there is no “off-switch” to this production of spike protein, but I do not currently have a citation showing this to be accurate. In any event, the effect of spike protein production should be considered.
The odd response is the production of 2 types of antibodies. This includes antibodies like IgG that fight the infection and also binding antibodies (not necessarily involved in preventing future infection. These binding antibodies may cause your immune system to worsen, instead of improve. If the vaccine instructs the body to make this spike protein and in turn the 2 types of antibodies, this could be problematic especially if the binding antibodies are produced as a large percentage of the total antibodies
Anyone who has taken the COVID-19 shots may want to consider an active natural medicine program to help to build and support their immune system.
The bottom line: at this time, it does not see that this strain of candida would cause concern for people who are currently healthy. Keep your gut microbiome healthy, be sure you get healthy sleep and try to get to bed by 10pm each night. Eat right by eating whole, unprocessed foods that support your digestive health and ultimately your immune system health. Remember that refined sugar can suppress white blood cell production for up to 6 hours. Keep doing practices that will build your immune system. Always remember that it is much less about the particular pathogen to be concerned about (like the candida) and much more the terrain of your body (gut microbiome, stress level, toxic load, exercise habits and more).
Ariel Policano is a naturopathic doctor specializing in energy medicine, frequency technologies and principles of nature cure. Learn more at her YouTube Channel, @arielpolicano and at geniusbiofeedback.com